- Introduction to Subjective Methods
- Birth weight
- Body shape
- Weight and height
- Waist and hip circumference
- Introduction to Objective Methods
- Simple measures - stature
- Simple measures - weight
- Simple measures - circumference
- Simple measures - arm anthropometry
- Simple measures - skinfolds
- Simple measures - abdominal sagittal diameter
- Simple measures - head circumference
- Bioelectric impedance analysis
- Multi-component models
- Hydrostatic underwater weighing
- Air displacement plethysmography
- Hydrometry
- Whole body DEXA scan
- Near infrared interactance
- Whole body counting of total body potassium
- 3d photonic scan
- Magnetic resonance imaging (MRI) / Magnetic resonance spectroscopy (MRS)
- Total body electrical conductivity (TOBEC)
- Computed tomography (CT)
- Ultrasonography
- Introduction anthropometric indices
- Body mass index
- Fat and fat free mass indices
- Ponderal index
- Percentiles and Z-scores
- Anthropometry Video Resources
- Height procedure
- Protocol for measuring waist circumference
- Measuring hip circumference
- Weight and body composition procedure
Simple measures - circumference
Body circumferences reflect internal (visceral, paravertebral and intermuscular) and subcutaneous adipose tissue, but are also influenced by variation in lean and bone masses. The inference made from a measure of circumference varies by anatomical site:
- Upper-arm, chest, waist, hip, med-thigh, calf and neck circumferences are generally used to describe fat distribution as well as predicting body fat
- Calf, thigh and upper arm circumferences are also used to estimate changes in musculature/lean mass and are strongly influenced by variation in appendicular skeletal muscle.
- Waist and hip circumferences are measures of "abdominal girth", the circumference around the midriff of the body. These measures are used in the assessment of central adiposity, which strongly correlates with cardio-metabolic disease risk.
Measures of circumference can also be combined:
- When waist circumference is used together with hip circumference (waist to hip ratio) it is indicative of the masculine (upper body) or feminine (lower body) distribution of adiposity.
- People with a high waist to hip ratio ("apple shaped" individuals) are more at risk of metabolic disorders such as obesity and diabetes than those who have a low waist to hip ratio (the "pear shaped" individuals).
- Waist to calf ratio or waist to thigh ratio, strongly predict sarcopenic obesity, typically found in middle age and older individuals as lean mass gradually decreases with age even if body fat remain unchanged or slightly increases.
Instrumentation
Different measurement tapes are available to measure circumferences. Typically a non-stretch (e.g. fibreglass or plastic), flat, flexible, ergonomic, measuring tape is used (see Figure 1 for examples).
Precision is generally improved by using a tape that maintains a fixed tension with spring attachments or else contains a tension indicator, since this minimises intra- and inter-observer variation in the extent to which the tape is pressed onto the participant during measurement.

Figure 1 Examples of tape measures (D-loop and tape measure with spring attachment).
Source: MRC Epidemiology Unit
The instrument needs to be calibrated using a standardised one-metre rod, especially when using plastic coated fabric measurement tapes as they may stretch with use overtime introducing error. It is common practice to carry out calibration procedures on a monthly basis.
Procedures
- Typically participants are standing up for the measurements of circumferences, unless measuring infants. Refer to each procedure
- Observers should be aware of the potentially sensitive nature of this measurement and take appropriate steps to minimise participant anxiety.
- Clothes introduce error into any circumference measurement so should be limited as much as possible while taking into account participant discomfort. Ideally, measurement should take place in underwear, but in practice a satisfactory measurement may be taken by removing outer layers of clothing, such as jackets or sweaters, and taking the measurement over light clothing (e.g. one thin layer of clothing)
- The use of a mirror is recommended to ensure accurate tape placement
- The observer to ensure reading is taken from outside the edge of buckle if using a D-loop tape measure
- Measurements are recorded to the nearest 0.1 cm (1 mm)
- Three measurements are typically recorded. The mean is derived by adding the values together and dividing by the number of measurements
Procedure for upper arm
- The circumference is taken at the mid-point between the bony protrusion on the shoulder (acromion) and the point of the elbow (olecranon process). The observer is to locate this midpoint in the non-dominant arm, with the participant’s elbow to be flexed 90 degrees with palm facing upwards.
- Participant to stand straight with arms hanging freely at the side and the palms facing the thighs.
- The tape should pass through the two landmarks and the midpoint marked.
- The tape is snug, not too tight (compressing the skin) or too loose, lying flat on the skin, and is horizontal (parallel to the floor). If measuring infants, the measurement is taken as the infant lies on the back or on their parents/carer's lap.
Procedure for chest
- The measurement is taken at the level of the middle of the sternum (breastbone), with the tape passing under the arms (see Figure 2). Once the tape has been positioned, the arms are then relaxed by the side, and the measurement is recorded at the end of a normal expiration as the position of the diaphragm could influence the accuracy of the measurement
- The tape is snug, not too tight (compressing the skin) or too loose, lying flat on the skin, and is horizontal (parallel to the floor). If measuring infants, the measurement is taken as the infant lies on the back
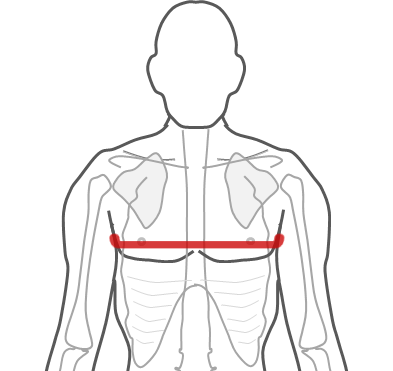
Figure 2 Chest – tape placed at the level of the middle of the sternum (breastbone).
Source: MRC Epidemiology Unit.
Procedure for mid-thigh
- This measurement is usually taken in the non-dominant leg
- Thigh circumference is measured perpendicular to the long axis of the thigh at the midpoint between the inguinal increase and the proximal border of the patella – the top of the patella
- When recording, the tape is snug, not too tight (compressing the skin) or too loose, is lying flat on the skin, and is horizontal
- If measuring infants, the measurement is taken as the infant lies on the back or on their parents/carer's lap
Procedure for calf
- This measurement is usually taken in the non-dominant leg. The participant is standing straight, feet approximately 20 cm apart, body weight equally distributed on both feet, and the measurement is recorded at the level of the widest circumference of the calf (between the base of the patella and the ankle).
- The tape is snug, not too tight (compressing the skin) or too loose, lying flat on the skin, and is horizontal (parallel to the floor).
- If measuring infants, the measurement is taken as the infant lies on the back or on their parents/carer's lap.
Procedure for neck
- This circumference is taken at the halfway point between the collar bone and chin (at the point of the larynx) with eyes focused straight ahead
- The tape is snug, not too tight (compressing the skin) or too loose, lying flat on the skin, and is horizontal (parallel to the floor)
Procedure for waist
- Participant is standing upright with feet slightly apart and arms hanging loosely to the side
- The measurement is taken at the end of a normal expiration as the position of the diaphragm could influence the accuracy of the measurement
- The World Health Organisation STEPS manual recommends taking this measurement in individuals in a fasted state to reduce the effect of stomach content
The site of WC measurement varies by study group as to date no consensus has been agreed on an optimal location. All measurements are taken along the horizontal plane, parallel to the floor. Whichever site is chosen should be used consistently for all measurements in any single study or survey group.
The most commonly used sites are:
- The midpoint between the lower coastal region (lowest palpable rib) and the top of the iliac crest, as used in the World Health Organisation STEPS manual for both children and adults, although no case is made in the manual as to its superiority to other sites.
- The upper border of the iliac crest (top of the pelvic bone).
- The narrowest part of the waist, as advised by the Anthropometric Standardization Consensus Group Source [ (Lohman et al, 1988).
- The lower costal margin (lowest rib).
- The upper border of the iliac crest (suprailiac crest) as used by the US National Institute of Health for identification of central obesity.
- The umbilicus (‘belly-button’), navel (generally 1 or 4 cm above the umbilicus) as used by the US National Institute of Health for identification of central obesity in the Multi-Ethnic Study of Atherosclerosis.
All sites are highly reproducible even though the waist values themselves may differ greatly from site to site (Source [10]). Differences in measurements protocols across studies could be responsible for variation in the association of these measures with risk factors, or disease or mortality outcomes.
This presents a particular challenge for anyone attempting to harmonise waist circumference data from multiple studies obtained from different anatomical sites. It also emphasises the need for rigorous standardisation of methods in multi-centre studies or surveys, since use of multiple sites will introduce measurement error.
The protocols with the bony land marks are preferable to the soft tissue landmark, such as the umbilicus, as many individuals with obesity may present pendulous abdominal adipose panniculus (dense layers of subcutaneous fat tissue in the lower part of the abdomen), resulting in the umbilicus to be located well below the waist level. The panniculus may also interfere with the hip measurement as the waist and hip circumferences overlap.
- Before locating the anatomical sites on the study participant, the observer to kneel or be seated on a stool, slightly to one side of the participant, since this allows better viewing of the results while minimising participant discomfort.
- The observer to feel for the anatomical sites (e.g. lower rib margin (costal margin) and for the iliac crest if using the WHO protocol Figure 3). It is recommended to ask the participant to mark both sides with their fingers when the measurement site has been located.
- Participant to have the arms by the side and relaxed, looking straight ahead.
- The observer to ensure that participant does not deliberately hold themselves in or out.
- The tape is snug, not too tight (compressing the skin) or too loose, lying flat on the skin, and is horizontal (parallel to the floor).
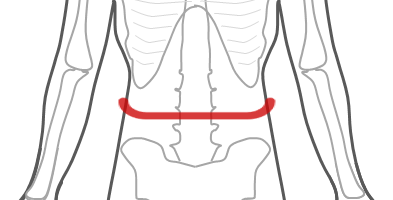
Figure 3 Waist – midpoint between subcostal and suprailiac landmarks according to the World Health Organization (WHO) protocol.
Source: MRC Epidemiology Unit.
Procedure for hip
- Participant will be standing upright with the arm relaxed at the side, heals together, and all the objects from pockets removed if measuring over clothing.
- To identify the hip, the observer to ask the participant to rotate their foot. The tape is positioned at the widest level of the buttocks, over the trochanters (the bony projections on the side of the femur). If the panniculus is present due to obesity and the waist and hip circumferences overlap, the observer to ask the participant to lift the extra tissue and place the tape under the panniculus and to measure at the largest circumference of the buttocks.
- The tape is wrapped snugly around the participant, but not to the point that the tape is compressing the skin. Keep the tape level and parallel to the floor at the point of measurement.

Figure 4 Hip – tape placed on the greater trochanter (bony projection on the side of the femur).
Source: MRC Epidemiology Unit.
Circumferences are commonly used in a variety of health related studies and in large scale epidemiological studies to assess central adiposity and fat distribution as they correlate with metabolic markers and imaging techniques estimates.
Waist circumference and BMI measurements are highly correlated with each other, at least in children above the age 5 years (R2 = 56% at 3.5 y; R2 = 61% at 4 y; R2 = 66% at 5 y; R2 = 75% at 7 y; R2 = 79% at 8 y; source: Avon Longitudinal Study of Parents and Children).
In clinical practice, this circumference would not add much to BMI to distinguish which children are overweight. However, at younger age groups, waist measurement may potentially provide additional information beyond BMI.
In research settings, simple measures like waist and hip other than BMI and weight may help understanding the causes of adiposity and assess intervention with longer term benefits.
Measurements should be quality checked during data processing in the same manner as other health related variables, for example by checking for outliers and data entry errors. It is recommended to use valid ranges for these circumferences according to the study population (e.g. children, adults etc.) when building the study database.
There are no specific steps, which are unique to these measurements. In some circumstances, it may be necessary to convert units taken in imperial units (inches) to metric units (cm).
Circumference ratio indices
Circumferences are often used in combination with each other or with other anthropometric measurements such as height, to calculate anthropometric ratio indices. This requires the division of two numbers (e.g. 2 circumferences or one circumference and one other anthropometric measurement) in the same units to derive the following ratio indices:
- Waist-to-hip ratio
- Waist-to-calf ratio
- Waist-to-thigh ratio
- Waist-to-height ratio
Waist and hip values as well as their ratio can be interpreted using population specific cut-off points.
Table 1 highlights the "at risk" categories in Europid using waist circumference and waist-to-hip ratio according to the World Health Organisation STEPS manual.
Table 1 Risk categories for waist circumference and waist-to-hip ratios.
| |
|
At substantial risk |
|---|---|---|
| Men |
|
|
| Waist circumerence |
≥ 90 cm (in South Asian, Japanese, Chinese) |
|
| Waist/hip ratio |
|
|
| Women |
|
|
| Waist circumerence |
|
|
| Waist/hip ratio |
|
|
Adapted from: WHO and Zimmet &Alberti (2006) Source [1, 15].
An overview of the characteristics of circumference methods is outlined in Table 2.
Strengths
- Inexpensive.
- Non-invasive.
- Limited burden to participant.
- Limited burden to researcher in terms of collection and analysis.
- Requires no input by participant and as such no risk of respondent biases.
- Used for a wide range of anthropometric ratio indices.
- Simple markers of adiposity.
- Waist and hip circumferences cut-off points to estimate obesity related health risks are available for different ethnic groups (South Asian, Japanese, Chinese and European).
- Circumferences ratios like waist-to-height ratio found to be better at predicting CVD risk factors than BMI. Waist-to-height ratios vary only slightly by age and by sex among children, it is not necessary to express measures as percentiles or Z-scores, relative to a reference population, as is the case for BMI. Simpler calculations than BMI as only requires the division of numbers in the same units.
Limitations
- These measures are poor at discriminating visceral from subcutaneous fat regions.
- They are characterised by low accuracy and reproducibility.
- Can be challenging to identify the correct anatomical site for the measurement, especially in obese individuals.
- Tension on the tape can affect reliability.
- They are subject to intra- and inter-observer variations.
- Measurement error is high.
- Wrapping the measuring tape too tightly or too loosely could result in an erroneous estimate and observer variability.
- The waist measurement depends on muscle mass, bone structure, laxity of abdominal muscles, fasting vs. postprandial state, phases of respiration, and posture of the individual. Stomach contents at the time of this measurement can also influence the values and introduce errors.
- Standardisation of protocols, especially for waist circumference are not always available, making comparisons and harmonisation across studies challenging.
- Lack of reference data in children, where reference data available, only appropriate for a specific site location (e.g. umbilicus level in children).
- Great inter-ethnic variability exists with circumferences and cut--off values are not always available for different populations.
- Indices more prone to measurement error because two measurements are required.
- Indices are more complex to interpret than circumferences, since increased ratios can be caused by increased fat or decrease in muscle mass.
- Turning the measurements into a ratio leads to a loss of information: two people with very different BMIs could have the same waist-to-hip ratio.
Table 2 Characteristics of circumference methods.
| Consideration | Comment |
|---|---|
| Number of participants | Large |
| Relative cost | Low |
| Participant burden | Low |
| Researcher burden of data collection | Low |
| Researcher burden of coding and data analysis | Low |
| Risk of reactivity bias | No |
| Risk of recall bias | No |
| Risk of social desirability bias | No |
| Risk of observer bias | Yes |
| Space required | Low |
| Availability | High |
| Suitability for field use | High |
| Participant literacy required | No |
| Cognitively demanding | No |
Considerations relating to the use of circumference methods in specific populations are described in Table 3.
Table 3 Use of circumference methods in different populations.
| Population | Comment |
|---|---|
| Pregnancy | Suitable, but measurements may not be reliable as unable to disentangle the maternal-fetal unit. Challenging to obtain these measurements in the last trimester as it might be difficult to identify the correct landmarks. |
| Infancy and lactation | Suitable, but no reference data available (see further considerations). |
| Toddlers and young children | Suitable, but no reference data available (see further considerations). |
| Adolescents | Suitable. |
| Adults | Suitable. |
| Older Adults | Suitable, but oedema may affect the ability to obtain reliable measurements especially in the leg region. |
| Ethnic groups | Suitable, but cut-off values not always available for different populations. |
| Other (obesity) | Suitable, but accurate measurements difficult to obtain as measurement locations are not always identifiable due to increase in soft tissue. |
It is recommended to estimate the technical error of measurement to monitor intra- and inter-observer variation.
Refer to section: practical considerations for objective anthropometry
- Measurement tape (in cm)
- Data entry form in either paper or computerised form
- Trained research staff, two required for certain measures
- Standard operating procedures for data collection
- Standard operating procedures for data entry errors/extreme values/data cleaning
A method specific instrument library is being developed for this section. In the meantime, please refer to the overall instrument library page by clicking here to open in a new page.
- Alberti KG, Zimmet P, Shaw J. Metabolic syndrome--a new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabetic Medicine. 2006; 23(5);469-80
- Agarwal SK, Misra A, Aggarwal P, Bardia A, Goel R, Vikram NK, et al. Waist circumference measurement by site, posture, respiratory phase, and meal time: implications for methodology. Obesity. 2009;17(5):1056-61. Epub 2009/01/24.
- Bray GA, Bouchard C, James WPT. Handbook of Obesity: Volume 1: Etiology, and Physiopathology. Number 2 ed: Taylor & Francis Ltd, CRC Press; 2007.
- Freedman DS, Kahn HS, Mei Z, Grummer-Strawn LM, Dietz WH, Srinivasan SR, et al. Relation of body mass index and waist-to-height ratio to cardiovascular disease risk factors in children and adolescents: the Bogalusa Heart Study. The American journal of clinical nutrition. 2007;86(1):33-40. Epub 2007/07/10.
- Hsieh SD, Muto T. The superiority of waist-to-height ratio as an anthropometric index to evaluate clustering of coronary risk factors among non-obese men and women. Preventive medicine. 2005;40(2):216-20. Epub 2004/11/10.
- Kim SK, Choi YJ, Huh BW, Kim CS, Park SW, Lee EJ, et al. Ratio of waist-to-calf circumference and carotid atherosclerosis in Korean patients with type 2 diabetes. Diabetes care. 2011;34(9):2067-71. Epub 2011/07/22.
- Klein S, Allison DB, Heymsfield SB, Kelley DE, Leibel RL, Nonas C, et al. Waist circumference and cardiometabolic risk: a consensus statement from shaping America's health: Association for Weight Management and Obesity Prevention; NAASO, the Obesity Society; the American Society for Nutrition; and the American Diabetes Association. Diabetes care. 2007;30(6):1647-52. Epub 2007/03/16.
- Lu B, Zhou J, Waring ME, Parker DR, Eaton CB. Abdominal obesity and peripheral vascular disease in men and women: a comparison of waist-to-thigh ratio and waist circumference as measures of abdominal obesity. Atherosclerosis. 2010;208(1):253-7. Epub 2009/08/07.
- Mason C, Katzmarzyk PT. Effect of the site of measurement of waist circumference on the prevalence of the metabolic syndrome. The American journal of cardiology. 2009;103(12):1716-20. Epub 2009/06/23.
- Mason C, Katzmarzyk PT. Variability in waist circumference measurements according to anatomic measurement site. Obesity. 2009;17(9):1789-95. Epub 2009/04/04.
- Wijnhoven HA, van Bokhorst-de van der Schueren MA, Heymans MW, de Vet HC, Kruizenga HM, Twisk JW, et al. Low mid-upper arm circumference, calf circumference, and body mass index and mortality in older persons. The journals of gerontology Series A, Biological sciences and medical sciences. 2010;65(10):1107-14. Epub 2010/06/16.
- https://www.cdc.gov/nchs/data/nhanes/nhanes_07_08/manual_an.pdf
- https://www.nhlbi.nih.gov/files/docs/guidelines/prctgd_c.pdf
- https://www.who.int/teams/noncommunicable-diseases/surveillance/systems-tools/steps/manuals#:~:text=The%20STEPS%20Manual%20is%20comprised,help%20readers%20find%20specific%20topics.
- http://apps.who.int/iris/bitstream/10665/44583/1/9789241501491_eng.pdf
